08 Apr HIV Vaccine Closer Than Ever After New Trials Show Promising Results
After a new HIV vaccine showed promising results in initial clinical trials, researchers plan to partner with Moderna, manufacturers of one COVID-19 vaccine, to continue developing the innovative treatment.
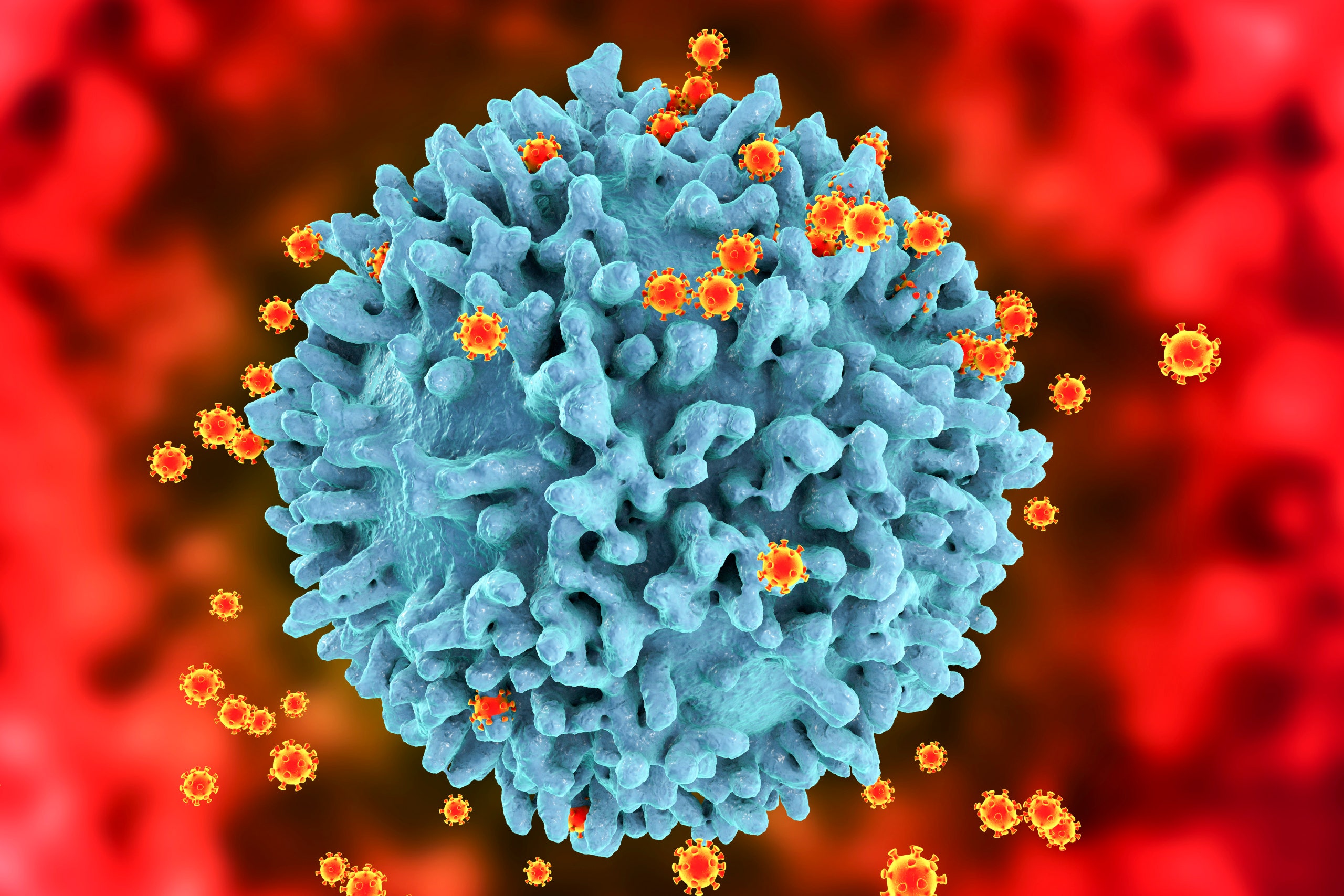
The experimental vaccine, developed by the International AIDS Vaccine Initiative (IAVI) and Scripps Research, displayed a 97% response rate among participants in an early stage Phase I trial, according to ABC News. Its novel approach involves stimulating the production of rare immune cells that are needed to start the body’s antibody generating process — a crucial step in combating the fast-moving virus.
Researchers say that using this technique to combat the HIV virus, which mutates rapidly and is notoriously hard to target with vaccines, could potentially accelerate the process of HIV vaccine development.
This approach is effective in targeting HIV specifically because the bnAbs could target a structural feature of the virus — its spikes — that does not differ much from strain to strain. If developed and approved, the vaccine, which primes the cells that create bnAbs, would be the first step in a vaccine regimen for targeting HIV.
HIV, which causes AIDS, affects more than 38 million people worldwide and disproportionately affects Black and Latinx people, as well as trans people. Because HIV targets and impairs the body’s immune response, people with HIV who are not on an effective course of antiretroviral treatment can be immunocompromised — putting them at greater risk of contracting COVID-19.
“This is a tremendous achievement for vaccine science as a whole,” said Dennis Burton, Ph.D., professor and chair of the Department of Immunology and Microbiology at Scripps Research, scientific director of the IAVI Neutralizing Antibody Center and director of the NIH Consortium for HIV/AIDS Vaccine Development in a press release.
Researchers involved in the vaccine’s development believe that it will have profound implications both for combating the global HIV epidemic and for vaccinology in general. “This study demonstrates proof of principle for a new vaccine concept for HIV, a concept that could be applied to other pathogens, as well,” added William Schief, Ph.D., a professor and immunologist at Scripps Research and executive director of vaccine design at IAVI’s Neutralizing Antibody Center.
Schief, whose laboratory developed the vaccine, presented the research at the International AIDS Society HIV Research for Prevention virtual conference in February. Researchers believe that the vaccine’s technique could be used to target other difficult viruses, including Zika, malaria, hepatitis C, and influenza.
Scientists and public health activists have drawn comparisons between COVID and HIV since the beginning of the pandemic, in comparing the successes and failures of the public health response to each virus. As is the case with HIV, Black and Indigenous people are more likely to contract COVID-19 and are much more likely to be hospitalized or die due to the virus. Recent research has also shown that LGBTQ+ people of color are far more likely to get COVID than their white counterparts.
The rise of PrEP as a method of HIV prevention and new treatments for those living with HIV have given advocates hope that a cure may be closer than ever. But in recent years experts have noted that progress in decreasing HIV infections has “stalled,” and a recent report pointed to increasing rates of the virus among trans people.
This plateau may be in part to a lack of access and usage of PrEP among affected communities; studies show widespread barriers to access and misinformation about the treatment, which has proven to be highly effective at preventing HIV. The drug’s high price point — it can run up to $2,000 a month — is also an issue that has attracted criticism and protest from AIDS advocacy group ACT UP and others.
HIV is still considered to be a global epidemic by the WHO.


